On Primary Care
General Practice, Pharmacy, Workforce
COVID-19 update
The articles that make up On Primary Care: General Practice, Pharmacy, Workforce were prepared shortly before the UK went into ‘lockdown’ to slow the spread of COVID-19.
This means that our authors had not, at that time, had to deal with the global COVID-19 pandemic and the scale and intensity of the new challenges posed to our healthcare system.
With that in mind, we asked our contributing authors to write their own short reflections on where the COVID-19 pandemic has impacted upon the current operation of primary care, and where the experience of the outbreak and our response is likely to influence longer-term policy thinking in these areas.
In this short addendum, we present reflections on COVID-19 and:
- Primary Care Networks
- Health and Wellbeing Boards
- Integrated Care Systems
- Pharmacy
- Workforce
We hope that these preliminary reflections shed some valuable light on the ways in which the primary care policy agenda will need to adapt to the new and disrupted environment in which our healthcare sector finds itself today.
Policy@Manchester
Primary Care Networks
NHS England was quick to respond to the pandemic, with the early publication of new Standard Operating Procedures for General Practices. This mandated remote access to primary care and set out procedures for using Personal Protective Equipment etc. The roll out of the Primary Care Network contract was also modified, with delay in the introduction of the service specifications and a blanket provision of the Investment and Impact Fund incentive monies to all PCNs without the need to meet the relevant targets.
It is clearly too early to tell how the PCN programme has been impacted by the pandemic, but two issues seem pertinent for further consideration as the dust settles. Firstly, it will be very interesting to explore whether and how PCNs have played a role in the response to the virus. PCNs have been promoted as one of the solutions to our current primary care workforce and access crisis, supporting collaborative working and the employment of a wider variety of types of practitioner. A crisis such as this would seem to be a good test of that proposition. Have areas with well-developed inter-practice collaborations fared better in the crisis?
The second interesting question is the reciprocal of this. How has the pandemic affected the development of PCNs? The lockdown occurred just as PCNs were absorbing the contract changes and considering how they would tackle the various service specifications. This work will have been halted to accommodate the urgent work needed to provide pandemic-related care. Recruitment of new practitioners may also have been halted, as current and future staff were mobilised and redeployed to support acute care. Finally, whilst the service specifications as a whole were paused, in April 2020 Simon Stevens announced that the Enhanced Health in Care Homes service specification was to be accelerated to provide additional support for the struggling Care Home sector. This provoked consternation amongst GPs, who were themselves struggling to provide care in unprecedented circumstances.
As primary care recovers from the first phase of COVID-19 and prepares for a possible second wave over the winter, Primary Care Networks should have an important role in supporting co-ordination between practices and providing mutual help in navigating the changing circumstances. Providing existing and (hopefully) new vaccinations, supporting Care Homes, and helping with ‘test and trace’ operations will all require primary care to be flexible and to work closely with other sectors; if they work well, PCNs will be the ideal vehicle to help make these things happen.
Health and Wellbeing Boards
It has become apparent that the risks from COVID-19 are further exacerbated by social and economic inequalities, and issues linked to ethnicity, gender, age and underlying health conditions. The strength of developing place-based initiatives in England is that they focus on the impact of the wider determinants of health (housing, employment, transport etc.), not just ill-health (in press) and HWBs are uniquely placed to help align policy and provide strategic direction in a place setting. In addition the pandemic has exposed the fragilities of the health, social care and public health systems in England.
According to the Local Government Association, Health and Wellbeing Boards have not generally met during the COVID-19 crisis. A HWB “is not an operational arm of place” and the majority of HWB members (including Directors of Public Health, Directors of adult social care, CCG accountable officers, acute CEOs) were fully engaged in frontline and emergency responses. With the immediate crisis coming to an end, HWBs will have an important role to play in the recovery of local systems.
There will be a challenging path to navigate between the need to re-evaluate priorities in the context of the pandemic (updating the Joint Strategic Needs Assessment and Joint Health and Wellbeing Strategy), making plans to reduce the health and other inequalities exposed during the last few months and short term action required to avoid subsequent potential waves of the virus, all in the context of the difficult financial environment. Future integrated working between organisations and sectors will be key to recovery and sustainability of local healthcare economies and the communities they serve.
Integrated Care Systems
The coronavirus pandemic has provided an early test for existing and developing Integrated Care Systems (ICSs). The programme of designating areas as ICSs has continued through the pandemic, with four new Systems named in May. There is some consensus that ICSs have been very important in the corona virus response, and that the experience of working together to solve the myriad of problems arising from the need to rapidly re-engineer care in all sectors has led to a new appreciation of their value and role.
In our pre-COVID assessment of the role of ICSs we highlighted the need to consider a more formal statutory underpinning for them, and it would seem that emerging ICS leaders agree, with an increasing proportion of ICS leaders telling the Health Services Journal that they feel that status as a formal statutory body will be important in the future. It also seems likely that the huge problems associated with the growing backlog of elective hospital care will need to be addressed at ICS rather than individual provider level, with pooled waiting lists and cooperation between hospitals. This would suggest that the era of care provided by competing independent Foundation Trusts is finally over; what this will mean for patient choice remains to be seen.
It would seem that the need for a co-ordinated response to the pandemic has probably accelerated the development of ICSs. However, as the emergency eases, careful attention will need to be paid to governance and accountability and to ensuring that all voices are heard.
Pharmacy
Community pharmacies experienced considerable additional demands on their services in the early weeks of the COVID-19 lockdown. At a time of great need, community pharmacies were one of the few healthcare providers that remained open for urgent care and advice. Indeed, additional funding made it a requirement for pharmacies to remain open over the Easter and early May bank holidays.
One of community pharmacy’s core functions remained the continued and safe supply of medicines, including to patients living in care homes. Pharmacies were funded to provide a medicines delivery service for shielding patients whose medicines could not be collected. This funding will end at the end of July, and whilst many community pharmacies offer medicines delivery services, these are not normally funded.
The COVID-19 pandemic has seen increases in electronic transfer of prescriptions and electronic repeat dispensing, thus avoiding the need for personal contact and paper prescriptions, and accelerating progress towards a paperless NHS. In cases where prescriptions could not be obtained, pharmacists could use already existing mechanisms, such as emergency supplies, to secure continued access to prescription medicines. Further contingency legislation was made for the supply of controlled drugs during a pandemic, and this can be activated if needed.
As the health service will remain under considerable pressure, community pharmacies offer the potential to provide acute care and become further integrated within NHS111 referral. Community pharmacies’ role in public health can be built on further, including virus testing and COVID-19 vaccinations when available. There is a particular opportunity to recognise pharmacies as assets within their communities and maximise their contribution to addressing health inequalities, which has particular relevance in relation to COVID-19.
Moving forward, it is essential that the positive changes to pharmacy practice are not lost in the wider recovery from the coronavirus pandemic. Community pharmacy will be able to play a constructive role in servicing the pent-up demand for everyday medical treatments that have been put on hold during the acute phase of the pandemic. To do so, however, it must be properly supported, integrated into our local healthcare systems, and recognised as a central, front-line service with a vital role to play.
Workforce
Across the UK, primary care responded to the coronavirus pandemic in various innovative ways by increasing use of telephone and video consultations, collaboration between practices to establish separate services for suspected COVID-19 cases, and remote working. While the extent to which practices continue with or reverse the shift to remote working remains unclear, some have predicted that the landscape of general practice has permanently changed.
During the crisis, the healthcare workforce was strengthened by re-registration of healthcare staff who had left the NHS and early deployment of final year medical and nursing students. However, there are indications that up to 20% of the health and social care workforce may leave after the crisis has passed and it is unclear whether returning workers will remain.
Overall, fewer consultations took place during the national lockdown and there was a marked and sustained decrease in urgent and routine referrals. It appears likely that primary care services will be significantly stretched due to these delays alongside continuing physical and mental health problems arising from the pandemic.
Contributing authors
Professor Kath Checkland Institute for Health Policy and Organisation
Professor Ellen Schafheutle Centre for Pharmacy Workforce Studies
Dr Anna Coleman Institute for Health Policy and Organisation
Dr Sharon Spooner Institute for Health Policy and Organisation
Foreword
Lord Keith Bradley
In the context of tightening budgets, organisational complexity, and the urgency of addressing the staggering inequalities of access and outcomes across the country, this is a time of unprecedented challenge for our health and care services.
Primary care is the public face of the NHS; the first point of contact for millions of men, women and children across the UK every day. It has become increasingly clear that, in order to cope with the invidious combination of rising demand and limited resources, it is essential to improve the quality, efficiency and effectiveness of these vital services.
The key for policymakers to achieve this, is integration. That is why I am pleased to introduce this new publication from Policy@Manchester, which sets out to address some of the biggest challenges of integration now facing the primary care sector.
This collection draws upon the formidable depth of expertise within The University of Manchester’s Faculty of Biology, Medicine and Health, with contributions from researchers affiliated with the recently-formed Institute for Health Policy and Organisation, the Centre for Pharmacy Workforce Studies, and the Alliance Manchester Business School.
This work is timely. The conversion of sustainability and transformation partnerships into integrated care systems is still underway, the primary care networks initiative still less than one year old, and the new contract framework for pharmacy was agreed only last year. On Primary Care delivers fresh and critical insight into the changes that are now taking place in our family surgeries, high street chemists, and clinics.
The articles contained within this volume, and the expertise of its authors, will be of great value to anyone involved in the creation, implementation, or scrutiny of primary care policy and practice.
I hope that each of these pieces, and On Primary Care as a whole, will make a full and substantive contribution to the ongoing development of the primary care sector, and improving the health and care services on which we all, ultimately, rely.
Lord Bradley was a member of the House of Commons Health Select Committee. As a peer, he has maintained a critical focus on health policy, including primary care, medicine, social care, with a particular commitment to improvements in mental health and learning disability services.

Primary care networks
The solution to our primary care crisis?
Dr Lynsey Warwick-Giles and Professor Kath Checkland

Multiple factors are contributing to a primary care crisis. There’s a serious workforce crisis, with general practitioners (GPs) leaving the profession and too few young doctors entering GP training. An ageing population is creating new challenges, with people living longer with multiple conditions.
In addition, there’s a growing public expectation of what the NHS should offer, and a mismatch between available funding and the cost of care provision.
What are primary care networks?
A variety of policy solutions have been proposed to address this complex crisis, most recently in 2019, with the introduction of primary care networks (PCNs) in the NHS Long Term Plan.
PCNs are essentially financially incentivised collaborations between groups of GP practices in a geographical area. They aim to create economies of scale by sharing administrative functions, resources and staff. They also are intended to work more closely with other community-based providers of care to create better, more joined-up services.
Recognising the urgency of the workforce crisis in primary care, initial funding for PCNs will concentrate on the employment of new types of workers across the PCN to improve delivery of services. In the first year, it will focus on the recruitment of social prescribing ‘link workers’ and clinical pharmacists, with a longer-term intention to recruit other new professionals such as physician associates and paramedics.
Over time, PCNs will be required to deliver new ‘service specifications’. These include more personalised care, better care for patients in care homes, and structured reviews for patients on multiple medications. In order to do this, PCNs will have to work more closely with other organisations such as community service providers.
Primary care networks - the story so far
Primary care networks have been established very quickly – in just three months. The process began in April 2019, with Clinical Commissioning Groups (CCGs) having to provide a list of PCNs and their associated practices by July 2019.
Primary care networks have been established very quickly – in just three months.
The registration process was light-touch. It required PCN member practices to complete and sign a network agreement, developed centrally by the British Medical Association (BMA) and NHS England, outlining PCN governance arrangements and how they should work together in general terms. Only at the end of this agreement is there a non-mandatory set of schedules, for PCNs to complete themselves, setting out the following important aspects of their operation in more detail:
- specific governance arrangements such as requirements to attend meetings and voting processes;
- how the PCN plans to work with other organisations;
- activities that the network will undertake;
- financial arrangements (who is receiving payments, for what activities, indemnities etc);
- workforce (how additional staff are being employed and supported);
- provisions for the insolvency of practices.
Networks did not need to complete these schedules in order to be registered, and some initially left them blank.
The mechanism by which PCNs have been established is contractual. Known as a ‘Directed Enhanced Service’ (DES), it is essentially an add-on to the General Medical Services contract for primary care providers. Practices volunteer to join a PCN, and in so doing become eligible for additional funding and support. The evolving five-year Contract ends in March 2024, with expectations and embedded incentives changing on an annual basis. Initial financial entitlements were set out in Summer 2019 and included:
- £1.50 per registered patient for each practice as a payment for participating (this is not new money; it will be provided by CCGs from their existing funding allocation);
- 100% of the cost of employing social prescribing link workers and 70% of the cost of employing other clinical providers, with the exact allocation for each PCN weighted to take account of deprivation and population demographics;
- funding for a Clinical Director at 0.25 FTE, per 50,000 patients.
Notably, there is no specific funding for management or administration beyond the Clinical Director post. Future funding from 2020/21 will include an ‘investment and impact fund’. This will be an incentive scheme, and will provide funding to PCNs for delivering objectives that are outlined in the NHS Long Term Plan and the DES.
PCNs will be required to meet a number of performance targets set out in a dashboard from April 2020. Indicators included were agreed by NHS England and the BMA and include data related to service specifications, population health and improvement, workforce and access and hospital use, as well as links to the investment and impact fund. However, exactly how this will work is not yet clear.
Long term challenges for primary care networks
The programme has already had a bumpy ride. Draft service specifications were put out for consultation just before Christmas 2019.
These addressed five areas:
- structured medication reviews and optimisation;
- enhanced health in care homes;
- anticipatory care;
- supporting early cancer diagnosis;
- personalised care.
Opposition from GPs and their representative organisations focused on the workload involved in delivering these specifications, and their inflexibility, with some GPs threatening to withdraw from the programme completely. NHS England quickly acknowledged that changes would need to be made, and these have subsequently taken place. On 6 February an update to the GP contract was published.
Significant changes to the DES have been made, including: increasing the funding allocated for new clinical professionals from 70% of the cost to 100%; the inclusion of a wider range of types of professional who could be employed; and the inclusion of an additional payment per patient living in a care home. Moreover, the expectations associated with the service specifications were significantly reduced. PCNs have fewer service specifications to deliver in 2020/21 (down from five to three) and the requirements associated with these have been scaled back.
Can primary care networks address this crisis?
PCNs are a crucial element in the ambitious commitments set out in the NHS Long Term Plan for a more integrated and joined-up system. The intention is that they will provide a voice for local services within new integrated care systems, and that they will form the focus of newly-integrated neighbourhood and community services.
Initially, there was considerable enthusiasm from GPs for PCNs, with a recognition that collaboration between practices is essential if they are to survive. However, there are a number of issues that NHS England will need to consider if the policy is to deliver long-term change.
Working together is never easy. Collectively employing staff and sharing funding will require robust and detailed governance and supporting processes. These will take time to develop. GP practices have worked together collaboratively before, for example in developing co-operatives to deliver out-of-hours care in the 1990s, and there is no doubt that such collaborations can improve job satisfaction for GPs. For PCNs to succeed, it is important that they are given time to develop the robust procedures and necessary trust for successful collaborative working.
While it is understandable that NHS England is keen for PCNs to start delivering some of the NHS Long Term Plan commitments quickly, the current workload pressures on practices should not be forgotten. We don’t yet know whether employing new workers will reduce demand on GPs, and some PCNs have struggled to recruit new types of staff. Delivering extensive and inflexible service specifications against this background is unlikely to be possible.
Funding mechanisms currently take limited account of demand or health inequalities. Delivering new services in areas of deprivation is likely to be more difficult, and this may need to be reflected in future funding. This may require, for example, incentive payments to be weighted to support practices in deprived areas.
Expecting PCNs to deliver changes in activity elsewhere in the system, such as A&E departments, is too ambitious. Any performance monitoring of PCNs will need to take existing workload pressures into account, as well as rising demand across the system.
Clinical Directors will be under considerable pressure, with multiple objectives to fulfil in limited time, and it is vitally important they are well supported. PCNs currently have no allocated funding for managerial or administrative support, and this requires credible plans for financing the administrative and managerial support that they will require to deliver on their objectives.
Belonging to a PCN is voluntary. If practices do not see any benefit in managing their ongoing workload pressures after the first year, there is a risk that they will choose not to participate.
If practices do not see any benefit in managing their ongoing workload pressures after the first year, there is a risk that they will choose not to participate.
If this happens, local CCGs would still be required to ensure that the patient population is able to access PCN services. This would mean the practices that have signed up may end up providing services for patients registered elsewhere, or the CCG would have to set up an alternative service.
It is clear that universal coverage will be more efficient and effective, and this has been reflected in the significant changes to the contract made during the negotiations. The next stages in the development of primary care networks are crucial, as practices settle down to delivering some of the additional work required.
Dr Lynsey Warwick-Giles is a member of the Institute for Health Policy and Organisation.
Professor Kath Checkland is a Professor of Health Policy and Primary Care at The University of Manchester. She is also Co-Director of the Institute for Health Policy and Organisation.



Place-based developments in health care
What can we learn from health and wellbeing boards?
Dr Anna Coleman

Health and wellbeing boards (HWBs) continue to be an integral part of the current health and social care system in England. They bring together a wide range of representatives from local organisations, build on local partnerships, and support joint working across sectors and organisations locally.
HWBs: the new system stewards?
The Health and Social Care Act 2012 gave HWBs specific functions, including the preparation of the Joint Strategic Needs Assessments and Joint Health and Wellbeing Strategies, both duties of local authorities and Clinical Commissioning Groups (CCGs).
With local responsibility for the strategic oversight of health care developments, and links with services which can have an impact on wider determinants of health, HWBs initially seemed ideally placed to become the new system stewards.
HWBs are sub-committees of upper-tier and unitary local authorities, made up of representatives from services across the NHS, public health, and social care, as well as children’s and other local services, including police, fire, voluntary and local healthwatch.
This configuration facilitated the potential for local cross-organisational work at a strategic level and provided the opportunity for longer-term development of collaborative working across the NHS and local government.
In 2016, we identified an ongoing struggle between local agendas, such as tackling inequalities, and central government priorities, such as integration, which suggested HWBs may only be a part of the solution. We recommended that they focus on their local system oversight and coordination roles in parallel with the development of local joint working practices.
Integration is seen by many as the solution to joint working, but the wider context of austerity and budget cuts, especially in local authorities, does not facilitate this. Additionally, constraints regarding organisational, professional and accountability rules and contexts continue to be problematic.
Our research suggested the role of HWBs remained unclear but had great potential to add value to and steer the local system.
Learning from the past
Partnerships (and other forms of integration) have long been mooted as a prerequisite for tackling complex issues that require a multi-agency response. Historically, however, they seem unable to break free from the silo-based structures which govern the organisation and delivery of many UK public services.
In 2019 I pointed out that there was potential to learn from HWBs in the context of developing integrated care systems (ICSs), evolving from sustainability and transformation partnerships (STPs) and suggested:
‘The new place-based system of working [following the publication of the 2019 NHS Long Term Plan] could usefully learn from [HWBs] how to operate successfully across sectors and organisational boundaries, include an element of democratic accountability, and create strategic partnerships of equals’.
This followed the publication of a report by the Local Government Association (LGA), ‘What a difference place makes’, which stated that ‘the original objectives for HWBs were as relevant to the new NHS landscape as they were in 2013, if not more so’. Their report highlighted work from 22 selected ‘well performing’ HWBs across England as illustrations of what can be achieved by working across local organisations to meet agreed strategic goals.
These were all published in advance of a King’s Fund report in 2019, which examined the ‘role of HWBs, and local government more broadly in relation to the emergence of ICSs’.
It suggested that: ‘There have been concerns that STPs have subsumed much of the work of HWBs but over a larger geographical area, so undermining the value of local place-based collaboration’.
‘Delivering together’, a paper from the NHS Confederation’s ICS network and solace in 2020, also pointed to the potential confusion and overlap of roles and responsibilities in the developing system:
‘HWBs have statutory responsibilities that include significant elements of the non-statutory roles of ICSs. Specific examples include oversight of commissioning plans, joint strategic needs analysis and responsibility for developing local strategies for health and wellbeing. This includes local authority-commissioned services such as social care and public health. Local authorities also have overview and scrutiny committees or sub-committees for health and care. These pre-date the Health and Social Care Act 2012 and can make recommendations to NHS organisations or central government, but do not have powers to require change’.
However, The King’s Fund report highlighted the unique input local government could potentially have by recognising the power of place in ICS development and the value of:
- collaborating at different levels in the system;
- building up from places and neighbourhoods;
- providing leadership across the system;
- focusing on functions that are best performed at scale.
HWBs, working at place level, have been piloting these local relationships through different types of leadership and collaborative ways of working since 2013, building relationships and associated trust within local systems.
As place-based working continues to be rolled out at a rapid pace across different levels (‘neighbourhood’, ‘place’ and ‘system’) in the health care system, the effective local work already carried out by HWBs should not be overlooked. Indeed, their experience of innovative joint working and work to shared strategic goals has much to offer.
Implications for ongoing policy development
‘Designing integrated care systems (ICSs) in England’, published in 2019, broadly set out the different levels of working within the developing ICSs, describing their core functions, the rationale behind them and how they will work together. This made only brief mention to HWBs, stating ‘ICSs will be expected to work closely with them, especially at the place-based level’.
By not highlighting the potential of HWBs in the local system, or detailing how these might actually operate together, is this a missed opportunity?
Contributors to the LGA report suggested that national conditions in the health care system have ‘caught up with the job HWBs were set up to do – in terms of highlighting the primacy of place, and of a partnership of equals’.
We should learn lessons from HWBs. They operate across organisations and sectors to facilitate the implementation of policy initiatives and help avoid contradictions and unexpected outcomes. One of the biggest problems with HWBs was lack of clarity about their roles and their lack of statutory authority. The way that ICSs are being established and operated could well be duplicating these same issues and consequent problems.
‘Delivering together’ goes further, voicing some of these concerns around the lack of clarity over roles and relationships, confusion over the interaction between the objectives of ICSs and other organisations and existing statutory duties, and uncertainty over the role and significance of ‘place’. It makes a plea for more careful thinking both nationally and locally as policies are rolled out.
The current speed of implementation of policies such as ICSs and primary care networks, following the publication of the NHS Long Term Plan in 2019 and associated initiatives at different levels, means we are in danger of losing the important lessons of history and the potential to build on what works in what context.
Dr Anna Coleman is a Senior Research Fellow in The University of Manchester's Division of Population Health, Health Services Research and Primary Care.



Integrated care
What's next?
Professor Kath Checkland

One of the most common complaints that people make about the care they receive from health and social care providers is that it is disjointed and fragmented, with different providers unaware of the others’ plans, and with recipients of care often forced to repeat their story many times. At the same time, both health and social care providers are under increasing pressure, and reducing duplication and working together more efficiently must be part of the long-term solution.
Current policy for integrated care
The NHS Long Term Plan, published in 2019, promised greater coordination and integration between health care sectors, and between health and social care. In primary care, the focus is on GP practices working together across a footprint of 30-50,000 people, coordinating and delivering services in collaboration with community services as primary care networks (PCNs).
Across larger areas, with populations between one and three million, integrated care systems (ICSs) are being created. These are intended to provide coordination between the wide range of care providers, and between commissioners and providers. They will act as a forum for this new scaled-up primary care to contribute to broader conversations. So far, so good, but can ICSs deliver?
It remains early days for ICSs. As of January 2020, there are only 14 ICSs in England, with a further 28 sustainability and transformation partnerships planning to move towards ICS status as soon as possible.
Greater Manchester is a little ahead of the game, having become the first devolved local authority in England in 2014. As well as having responsibility for housing, transport, planning, jobs, skills and wealth creation, health and social care became part of the deal in 2015, and the Greater Manchester Health and Social Care Partnership was formed. It brought together the Greater Manchester Combined Authority (GMCA), local commissioners, and major health care providers. Building on this, Greater Manchester was named as one of the first ICSs in England.
Lessons from Greater Manchester
Greater Manchester started with big ambitions focused around reducing health inequalities and improving health and wellbeing (aspirations which many developing ICSs will share). Perhaps inevitably, those ambitions have proved difficult to achieve, with an evaluation by colleagues at The University of Manchester concluding:
‘Those involved, especially at the outset, may have overpromised what devolution would achieve or the timescale in which changes would happen. We think this is well recognised by the Greater Manchester Partnership’s leadership which is now strongly focused on implementation.’
However, much has happened in Manchester under the banner of ‘Devo Manc’, and it provides a valuable case study from which other ICSs in England might usefully learn.
The value of trust and good local relationships cannot be over-estimated. NHS managers began working with GMCA well before devolution, and the relationship developed over many years, forming a strong base for the new collaboration. This raises issues for areas where such relationships haven’t historically been as close. Clearly you can’t retrospectively engineer better long-term relationships, but recognising any deficit and tackling obvious areas of conflict could be worthwhile.
Clearly you can’t retrospectively engineer better long-term relationships, but recognising any deficit and tackling obvious areas of conflict could be worthwhile.
The devolution project was rhetorically styled as ‘taking control’ of the £6 billion health and social care budget, but this was an overstatement of the case. Devolution did not involve any change to the existing statutory responsibilities for either health or social care organisations, and each organisation retained its pre-existing budgets and financial responsibilities. Anything that was achieved, therefore, was achieved using existing budgetary flexibilities and rules. This is important, as ICSs do not currently have any budget-holding powers and will need, just as Greater Manchester has, to negotiate and work collaboratively to achieve their goals.
An ICS governing body or board cannot, at present, allocate funds or shift resources, and they will need to establish mechanisms by which such decisions are made to take account of the statutory responsibilities of the individual organisations.
In Greater Manchester this was achieved, in part, by the establishment of some relatively elaborate governance arrangements, including the establishment of collaborative committees of commissioners and providers. Such arrangements take time to implement, and may require significant managerial support. Moreover, without statutory authority there is always a danger that, faced with difficult decisions, these carefully-built collaborative structures will collapse.
The Greater Manchester Health and Social Care Partnership did not take control of the full health and social care budget, but they did have some leeway over the spending of the region’s share of national ‘transformation’ funding. These funds amounted to £450 million, and were used, among other things, to establish cross-regional programmes such as a ‘workforce collaborative’, focused on ensuring the required health and care workforce is available in the future. Such cross-regional projects have been valuable in providing coordination and in creating a sense of purpose. It is worrying that current plans for ICSs do not seem to include any similar promises of discretionary spending. Even small amounts of such funding can be very helpful in supporting collaborative activity. This may be an area that national policy could address by allowing ICSs a small amount of discretionary development funding, for example.
The real work of integration in Greater Manchester is happening in the localities. On the commissioning side, collaborations between health and local authority commissioners at borough level are starting to plan more integrated care for their populations (approximately 200-300,000), while integrated provider organisations are starting to break down historical boundaries between sectors.
Primary care providers, working together in their new networks, are engaged in these discussions. This level – single local authority, a coherent local geography and providers who know one another – seems to be the level at which actual integrative activity can happen. The managers and care providers know each other and their populations, and are able to begin the difficult task of designing solutions to integration problems.
This level – single local authority, a coherent local geography and providers who know one another – seems to be the level at which actual integrative activity can happen.
However, this level is barely mentioned in the NHS Long Term Plan. Instead, it envisages just one single Clinical Commissioning Group (CCG) for each ICS. Given the size of ICSs (population one to three million, covering many local authority areas), it seems unlikely that one CCG will have the local knowledge and relationships which have been so important in galvanising locality integration in Greater Manchester.
Given the size of ICSs (population one to three million, covering many local authority areas), it seems unlikely that one CCG will have the local knowledge and relationships which have been so important in galvanising locality integration in Greater Manchester.
Strengthening the foundations of local health care systems
We would suggest the following policy priorities for ICS development across England;
Frank and forensic diagnostic work needs to take place in the early stages of each collaboration. Have these people worked together before? What problems did they have? What problems and misunderstandings need to be addressed? Those involved with the Greater Manchester experiment might have a useful role to play in providing candid accounts of what worked well for them, and what they found more difficult.
Strong collaborative governance structures are required, and may need to be put on a statutory footing. Prior to 2012, strategic health authorities (SHAs) had a statutory role in mediation between local commissioners and providers, and provided support where required. A more formally constituted ICS board could potentially play such a role.
A small amount of discretionary spending may be helpful in establishing meaningful collaborations. Dedicated NHS funding should be directly allocated to ICSs, allowing them to facilitate local collaborative activity.
Effective integration will require a strong structure at ‘place’ level. Local PCNs will need to work together across towns and boroughs to bring primary care together with other services provided across these ‘places’, and CCGs will have an important role to play in supporting them. If, as the NHS Long Term Plan envisages, CCGs are sto merge to form much larger organisations mirroring ICSs, they will need to develop strong internal structures to support PCNs. Such internal structures require staff who know their local area, and operating costs may not be as reduced as expected.
Taken together, these suggestions, all developed from our experience monitoring the evolution of local healthcare systems here in Greater Manchester, will provide evidence-informed improvements to the continuing roll-out of integrated care systems. If adopted, they promise to put ICSs on a more sustainable footing, with fairer expectations for performance and more capability to perform the functions that they have been designed for.
Kath Checkland is a Professor of Health Policy and Primary Care at The University of Manchester. She is Co-Director of the Institute for Health Policy and Organisation.



Community pharmacy in primary care networks
Integration for acute and urgent care
Professor Ellen Schafheutle and Dr Sarah Willis

As the population ages, health care needs increase, yet NHS resources are constrained. Policy is focusing on moving as much care as possible into the primary care sector, rather than hospitals. This approach is developing across our healthcare system, with health authorities across the UK all moving in the same direction.
Meeting the demand
General practitioners (GPs) who are experiencing severe workforce shortages cannot meet rising health care demands alone. Increased workforce diversification is one possible solution, together with an emphasis on self-care and patients taking responsibility for managing their own health needs, supported by a range of health care professionals.
The NHS Long Term Plan (2019) in England has recognised the contribution of pharmacy professionals to the primary care workforce. Investment under the Pharmacy Integration Fund (PhIF) has provided new roles for pharmacists as clinical professionals in a range of primary care settings, including general practice, care homes and urgent care settings, where they can practise as prescribers.
The contribution of community pharmacies is also recognised, and a new Community Pharmacy Contractual Framework (CPCF) was published in 2019. This builds on the changes to reimbursement in community pharmacy in 2005, which, while recognising the continuing medicines supply function of community pharmacies, introduced a number of funded clinical, medicines and public health services.
Community pharmacies’ contribution to acute and urgent care
The 2019 CPCF positions community pharmacies, which are already known for their accessibility (long opening hours, no appointments needed), as having a significant role in providing acute care for patients requiring short-term treatment.
Patients are less familiar with some of the public health and medicines services community pharmacies offer, but they do value pharmacists’ advice, and medicines sales and supplies for acute minor ailments.
This traditional role is to be extended considerably under the 2019 CPCF, emphasising community pharmacy as a first port of call, able to respond ‘swiftly, conveniently and effectively’ to patients’ acute and urgent (same-day) care needs. This aims to help address the significant pressures on higher-cost general practice and A&E departments by redirecting patients with minor ailments to community pharmacies.
This traditional role is to be extended considerably under the 2019 CPCF, emphasising community pharmacy as a first port of call.
The CPCF takes a phased approach to integrating community pharmacies as contributors to the urgent care agenda within primary care networks (PCNs).
The NHS Community Pharmacist Consultation Service is already being introduced, with community pharmacies receiving direct referrals from NHS 111. Referrals from other parts of the NHS, including general practice, are planned for the future. These referrals are either for an emergency supply of previously prescribed medicines, or to provide advice and/or over-the-counter medicine (available without prescription) to treat acute minor ailments, such as rashes, constipation, diarrhoea, vaginal discharge, sore eye, mouth ulcer, failed contraception, vomiting, scabies and ear wax.
The intention of the CPCF 2019, however, is for pharmacists to move beyond supplying urgently required medicines. They will conduct consultations, as well as notify the patient’s GP of any advice or support given, and/or medicines supplied. After some transitional payments in 2019/20, this will operate as a harmonised fixed fee of £14 per consultation.
What will be required to make this a success?
Community pharmacies need to become an integral part of PCNs. Effective collaboration between different NHS agencies and providers, via PCNs, needs to underpin the positioning of community pharmacies as the first port of call in NHS provision of urgent care services, with incentives for integration. This will address problems experienced, due to a variety of reasons, when general practice and community pharmacy have previously attempted to collaborate. GPs are keen to work with community pharmacies, provided joint working is of mutual benefit. This means that joint working, or working jointly towards the same outcome, needs to be incentivised. Yet the opposite can be the case, particularly with general practice and community pharmacy contracts traditionally designed and negotiated separately.
This means that joint working, or working jointly towards the same outcome, needs to be incentivised. Yet the opposite can be the case, particularly with general practice and community pharmacy contracts traditionally designed and negotiated separately.
Flu vaccinations in England, for example, can be offered as an NHS service in general practice or community pharmacy. However, initially there were problems with GPs not being aware their patients had been vaccinated in community pharmacy, and with the fact that GPs could not use these vaccinations towards their Quality Outcomes Framework points.
Policymakers should prioritise and, where possible, incentivise the development of IT infrastructure for two-way communication. Integration of community pharmacy into PCNs requires IT infrastructure that allows effective two-way communication for referrals (and their documentation) to and from community pharmacy. In the example above, it is important that GPs are aware if their patients have opted to receive their flu vaccination in community pharmacy. The importance of community pharmacists being able to view core information about patients’ current and discontinued prescribed medicines, as well as relevant allergies, when making an urgent medicine supply, for example, has already been recognised. Indeed, it is possible for community pharmacists to view this information in the summary care record (SCR).
To further develop this, promoting effective sharing of relevant information is key. A system (possibly linked to the SCR) could be trialled which allows some read/write access, while ensuring that appropriate safeguards exist to alleviate both public and GPs’ concerns regarding access to patients’ data by non-NHS, commercial organisations such as local/community and high-street pharmacies.
Building competence and confidence among community pharmacists will be a priority. For community pharmacies to be more integrated into PCNs means having a workforce with advanced clinical skills, allowing them to extend their scope of practice to the treatment and management of patients with more complex health care needs.
There is potential here for community pharmacy to build on improvements in providing access to treatment for underserved populations, covering an expanded range of conditions. Community pharmacists have already demonstrated change in practice following training, including changing their referral behaviours. The PhIF is currently offering training to support advanced practice training, and Centre for Pharmacy Workforce Studies (CPWS) will report evaluation findings in due course.
There is potential here for community pharmacy to build on improvements in providing access to treatment for underserved populations, covering an expanded range of conditions.
Pharmacists’ time needs to be freed for clinical interactions. As well as better integration within a PCN, the new contract signals an even stronger move for pharmacists away from medicines supply to more clinical activities enabled through diversification of the pharmacy workforce. Indeed, the NHS Long Term Plan has recognised this, and the PhIF is not only investing money in training for pharmacists, but also pharmacy technicians, enabling pharmacists to delegate more technical and dispensing activities.
While ensuring a highly-skilled pharmacy support staff workforce through appropriate training is important, our research has shown that there are other factors which need to be overcome to enable community pharmacy’s clinical contribution.
In hospitals, skill mix and role clarity enable pharmacists to deliver clinical care close to patients (on wards and in clinics), which is enhanced by pharmacists gaining prescribing qualifications. However, some community pharmacists appear reluctant to let go of traditional, more technical roles. It seems they do not fully trust support staff to fulfil these adequately, and practise more clinically, closer to patients.
Additional support, through leadership training and organisational change management, may be valuable (some of which is on offer under the PhIF) but workload and pressures also need to be addressed.
Our recommendations
PCNs and the new CPCF offer opportunities for community pharmacies to deliver high-quality patient care, and to be integrated with a range of health care providers.
One area of particular need is urgent care, where inappropriate consultations in general practice and A&E lead to pressures which could be alleviated through better use of an upskilled workforce in community pharmacy.
Inappropriate consultations in general practice and A&E lead to pressures which could be alleviated through better use of an upskilled workforce in community pharmacy.
The success of this redistribution of urgent care provision (best provider) will depend on:
- meaningful integration, supported by appropriate incentive structures;
- a shared IT platform to support this, not just to access limited and relevant information, but allowing the recording and two-way sharing of interventions;
- further training combined with support for organisational change within community pharmacy, to maximise the potential of pharmacy staff skills;
- establishment of a culture of evaluation, where increased recording of pharmacist interventions on shared platforms will link with patient outcomes.
Professor Ellen Schafheutle is the Director of the University’s Centre for Pharmacy Workforce Studies.
Dr Sarah Willis is a Lecturer in Social Pharmacy at The University of Manchester.



Quality matters in community pharmacy
Dr Ali Hindi and Dr Sally Jacobs

Maintaining and improving the quality of patient care is an NHS priority with the overall objective of achieving health care which is safe, effective, timely, efficient, equitable and person-centred.
The importance of quality in a growing field
The NHS has been at the forefront internationally for its quality improvement policies in primary care, notably, the implementation of a series of quality-improvement initiatives and the introduction of the largest health care ‘pay-for-performance’ scheme in the world, the Quality and Outcomes Framework (QOF) for GPs.
The QOF has been extensively researched since its implementation and there have been key developments, (most notably the role of the National Institute for Health and Care Excellence (NICE) in developing and reviewing indicators) over the years to ensure quality measures are developed in a systematic and transparent manner.
At the same time as expanding the role of primary care, the role of providers outside general practice has gained momentum. Community pharmacy is one established primary care provider with the potential to improve access for patients and relieve pressures on general practice. In 2019, the NHS Long Term Plan acknowledged that community pharmacy will have an even bigger role in urgent care and prevention, enabled by the Community Pharmacy Contractual Framework (CPCF). This introduces new pharmacy services over the next five years, which will integrate with other primary care settings through integrated referral pathways.
As the role of community pharmacy continues to expand, the need for ensuring high-quality services, meeting patient needs and integrating across patient primary care pathways has never been greater.
Primary care networks: an opportunity for quality through integration?
NHS England has made clear its intention to drive collaboration between general practice and other community-based providers, such as community pharmacy, in its Five Year Forward View (2014) and the NHS Long Term Plan (2019). Achieving better integration of general practice with other health
care providers could improve the quality of health care by ensuring patients receive timely, effective and efficient patient-centred care though clear referral pathways.
However, our recently published systematic review exploring the views of pharmacists and GPs on community pharmacy services (2005-2017) identified that GPs’ awareness of pharmacy services was low and collaboration between pharmacists and GPs was poor, despite the introduction of new pharmacy services intended to encourage joint working.
Moreover, a recent study involving GPs, community pharmacists and patients identified a lack of alignment between community pharmacy and GP contracts. This has led to competition over funding, rather than incentivised joint working to improve the quality of care for patients, for example in the case of flu vaccinations.
The study also found that GPs were supportive of community pharmacists providing some of the services traditionally provided by GPs (such as minor ailments and medicines reviews) to increase patient access and reduce workload pressures, but mentioned difficulties in collaboration due to interprofessional tensions arising from funding conflicts. For example, some GPs had advised patients to avoid using community pharmacies for flu vaccinations.
Recent developments have addressed some of these issues.
The introduction of primary care networks (PCNs) includes an obligation for general practice to work with other non-GP providers and community-based organisations, such as community pharmacies, to provide more joined-up care for patients. In light of this, the new community pharmacy contract has introduced quality payment incentives for pharmacies to collaborate with GPs and engage effectively with PCNs. In the GP contract, there is some acknowledgement of GPs working with community pharmacy as part of primary care networks. However, neither the community pharmacy nor GP contracts provide any specific guidance as to how community pharmacy teams will work closely with colleagues in general practice.
It therefore remains unclear how better integration between community pharmacy and general practice will be achieved in order to enhance quality of patient care.
Monitoring and ensuring quality in community pharmacy
The first big change to the reimbursement of community pharmacy occurred with the 2005 contract, which introduced a number of public health and medicines services, recognising the contribution of community pharmacy and its expanding role in primary care. Payment for these services was a ‘fee-for-service’ model, but there have been concerns over the quality of some community pharmacy services using this reimbursement model.
A major study carried out by the Centre for Pharmacy Workforce Studies (CPWS) highlighted that there was a positive culture in some pharmacies, encouraging the delivery of service quantity and quality by focusing on skill mix, team development and extended staffing models.
However, other community pharmacies were shown to prioritise quantity over quality of service delivery in order to maximise financial gain. In these pharmacies, high dispensing workloads and insufficient staffing levels led to dispensing duties being prioritised over medicine-related and public health services. In addition, management pressures to deliver a range of community pharmacy services led to increased waiting times, decreased clinical input, and increased risk of dispensing errors.
In the past decade, many approaches have been developed for measuring and assuring quality in community pharmacy, including new processes for:
- pharmacy regulatory inspections;
- contract monitoring and reporting;
- annual patient satisfaction questionnaires;
- error reporting and analysis.
However, our research suggests that quality measurement in community pharmacy is often opaque and variable, with little known about how widely implemented community pharmacy quality initiatives are, or how successful they are.
For example, there is no clear definition of quality in community pharmacy, and there is a lack of reliable and valuable methods for measuring service quality. When quality is measured, it is done using subjective informal mechanisms such as self-assessment by the pharmacy, patient feedback, GP feedback, and observed changes in a patient’s health or behaviour.
When quality is measured, it is done using subjective informal mechanisms such as self-assessment by the pharmacy, patient feedback, GP feedback, and observed changes in a patient’s health or behaviour.
In response to increasing concerns about a lack of quality measures or indicators in community pharmacy, NHS England introduced the Quality Payments Scheme in 2017, which aligns payment with value and quality by attaching financial incentives to provider performance.
Under the 2019 CPCF, the new scheme, renamed the Pharmacy Quality Scheme (PQS) has been revised with updated and retired indicators, as well as changes to the structure and content of the quality criteria.
The PQS promises to be a step towards tackling some of the problems around prioritisation of financial gain over patient care and encouraging engagement with PCNs.
As the PQS is in its early stages, the evidence around its implementation and effectiveness is sparse. Unlike the more established QOF for GPs, with a rigorous evidence-based process for selecting, piloting and evaluating performance measures, little is known about the process involved with the development of PQS indicators, or their effect on improving quality in terms of access, patient outcomes, or integration of community pharmacy within the wider primary care system.
Another approach may be to adopt a continuous quality improvement (CQI) programme such as the SafetyNET-Rx programme trialled in pharmacies in Canada, which offers payments for pharmacies that continuously and systematically examine work processes to identify and address causes of poor quality over time.
An evidence-based, collaborative approach to quality improvement
The NHS Long Term Plan seeks to improve patient care and relieve some of the pressures facing GPs by encouraging closer working with other health care organisations such as community pharmacies, although silo working still predominates in the NHS.
To optimise the potential of community pharmacy in meeting patient needs and alleviating workload pressures in general practice, there needs to be reassurance of the quality of care in this setting.
NHS England needs to ensure processes are in place for better integration between community pharmacy and general practice, which will translate into actions that improve service quality and patient outcomes. This requires aligning GP and community pharmacy contracts and providing more specific guidance as to how better joint working could be achieved via PCNs. It will be important to evaluate whether and how the PCNs, requiring pharmacies to collaborate with GPs, support effective integration.
Quality is still not well defined in community pharmacy, and systems for monitoring and improving quality are relatively underdeveloped. The evidence base for quality improvement in community pharmacy is insufficient. Research is required to develop valid and reliable evidence-based quality indicators (similar to QOF) which clearly demonstrate if and how community pharmacies are improving the quality of care in an integrated primary care system.
Dr Ali Hindi is a PhD researcher who has investigated the awareness, demand and use of community pharmacy services for patients with long-term conditions in the UK.
Dr Sally Jacobs is a Lecturer in Social Pharmacy at The University of Manchester.



Prevention in primary care
Community pharmacy in asset-based practice
Dr Jayne Astbury and Professor Ellen Schafheutle

Public health and prevention are now central tenets of NHS policy, yet health inequalities and social disparity in terms of ill health and reduced life expectancy persist.
The importance of community pharmacies
The 2010 Marmot Review drew attention to the social and economic costs of health inequalities and emphasised the role and importance of local government in addressing the social determinants of health. Access to NHS services, including general practice, is a well-established social determinant of health, with the most disadvantaged areas tending to have the lowest availability of services.
One exception to this trend is community pharmacy, with access being greatest in areas with higher levels of social deprivation. Their community-centric location, walk-in access, and extended opening hours make pharmacies a socially-inclusive and accessible health resource.
Their community-centric location, walk-in access, and extended opening hours make pharmacies a socially-inclusive and accessible health resource.
Their broad customer base includes individuals who are not necessarily in contact with other health care services, as well as those receiving regular or repeat prescriptions, creating a unique opportunity for pharmacies to offer both primary and secondary prevention services and support self-care.
Opportunities within the new Community Pharmacy Contract Framework
The 2019 Community Pharmacy Contract Framework (CPCF) recognises the ‘critical role of community pharmacy as an agent of improved public health and prevention’ and outlines continued support for public health services currently provided by community pharmacies, alongside the introduction of new services. The CPCF reflects the ambitions outlined in the NHS Long Term Plan to further utilise the skills and expertise of community pharmacy teams in achieving prevention, improved health outcomes, and medicines optimisation.
For this ambition to be realised, community pharmacists require the skills and confidence to adopt an increasingly patient-facing role and undertake patient-centred consultations. However, previous research suggests that pharmacists lack confidence in applying a patient-centred approach. Conversations with patients concerning self-care support tend to be medicine-focused, rather than patient-centred. Moreover, some pharmacists lack confidence in conducting consultations regarding patient-led goals and healthy lifestyle, and feel uncomfortable not using their medicines expertise. Barriers to adopting person-centred practices include professional identity, contractual frameworks, and a lack of incentives.
Prior to the recent development of the Pharmacy Quality Scheme (PQS), community pharmacy was reimbursed, and thus incentivised, for quantity or service volume rather than quality. Although the introduction of the PQS goes some way towards addressing this, the majority of community pharmacy delivery remains service-focused as opposed to patient-centred. While the pharmacy profession recognises the importance of adopting a person-centred approach, this has yet to be fully supported or implemented in practice.
Asset-based approaches to health and wellbeing
Traditional approaches to health and social care have typically focused on factors that contribute to ill health. Asset-based approaches focus on factors that support and promote good health and wellbeing by recognising and building on the strengths, skills, and assets that exist within individuals and communities.
Asset-based approaches focus on factors that support and promote good health and wellbeing by recognising and building on the strengths, skills, and assets
Assets in this context include any resource that supports individuals and communities to stay well. On an individual level this may include factors such as knowledge, life experiences and relationships. At a community level, assets may include physical resources such as green spaces, leisure centres and libraries, as well as less tangible resources such as local community networks and associations, and factors such as local culture, identity and skills.
Asset-based approaches seek to capitalise on these existing resources with an emphasis on connecting individuals to each other and to the broader ‘assets’ within their communities. Asset-based approaches are increasingly being used as a basis for public health initiatives and as a framework to support the integration of health and social care services.
The Centre for Pharmacy Workforce Studies (CPWS) recently explored the current and potential role of community pharmacy in asset-based practice. Research indicated that further adoption of this approach may enable community pharmacy to more effectively support the health and wellbeing of individuals and communities, and play a more central role in the reduction of health inequalities.
The study included interviews with public health and strategic leads, and community pharmacists. Public health and strategic leads were found to be supportive of community pharmacy’s role in asset-based practice. They highlighted the potential for this approach to inform and underpin public health work undertaken by the broader community pharmacy workforce, including health champions and pharmacy technicians.
The potential for community pharmacy to work collaboratively with emerging social prescribing initiatives that support people to access local non-clinical resources was also raised. Public health and strategic leads also highlighted the need for the community pharmacy sector to become more proactive in forging relationships and occupying roles within public health and primary care networks (PCNs).
Community pharmacists, on the other hand, conceptualised their current or potential involvement in asset-based approaches in terms of strength-based approaches to consultations and conversations with patients and customers.
They noted the contribution that pharmacies made, or could make, to their communities, beyond current standard commissioned services, including:
- collaborating with voluntary sector organisations in funding bids to develop community resources;
- providing space for community groups;
- supporting patients and customers to form peer support groups, such as walking groups.
Pharmacists recognised the need to have access to, and presence in, accurate locality asset maps or resource directories to enable pharmacy teams to effectively signpost customers to existing community resources.
The adoption of asset-based approaches was found to be influenced by a number of factors including the availability of time and resources, workplace and organisational culture and values, and commissioning and funding arrangements.
The role of Healthy Living Pharmacies
One suggested mechanism to support the adoption of asset-based practices included further development of Healthy Living Pharmacies (HLP). The CPCF stipulates that all pharmacy contractors will be required to reach level one HLP status, which aims to support them to proactively promote and influence health and wellbeing in their locality, by April 2020.
This means that all pharmacies will have trained health champions within the pharmacy team who are able to provide a range of interventions on key public health issues, in addition to offering self-care advice and signposting to other resources within the local community. Levels two and three of the HLP framework focus on commissioner-led services concerning prevention and protection, respectively.
The establishment of PCNs provides the opportunity to work towards commissioning public health and prevention services, including those provided by community pharmacies, that are more sensitive to local community needs.
Participants raised the possibility for further development of the HLP framework to include a component or level where a community pharmacy focused on engagement with, and contribution to, their local community, broadly aligned to the notion of social capital.
The findings suggested that community pharmacies would welcome additional support and guidance on how to make and increase their connections with, and contribution to, their community, and develop collaborative relationships with other services and sectors.
Community pharmacies would welcome additional support and guidance on how to make and increase their connections with, and contribution to, their community, and develop collaborative relationships with other services and sectors.
Integrating this type of activity into HLP was suggested as a potential mechanism for reimbursement and financial incentive. Some pharmacists, however, raised concerns regarding the current PQS and suggested that self-declaration could enable tokenistic engagement. They suggested commissioning and reimbursement should be aligned with a greater degree of independent scrutiny and evaluation to ensure quality is incentivised alongside engagement.
Policy implications
If community pharmacy is to achieve its full potential in relation to public health and prevention, there is a need for further integration of community pharmacy into local PCNs. The appointment of pharmacy PCN leads within each PCN locality, as encouraged within the CPCF, offers an opportunity for community pharmacy to be more effectively represented in local discussions concerning the ongoing development of PCNs.
Our research suggests that public health leads are keen for community pharmacy to develop a more substantial role in public health and prevention work. If this is to become a reality, the community pharmacy sector needs to take steps to proactively engage and develop collaborative relationships with public health and PCNs through the development of local and national strategic leadership roles.
It is clear that consideration of the potential role and value of integrating community pharmacy into emerging health initiatives, such as social prescribing, is warranted. Local commissioning of relevant HLP services may act as an initial mechanism to encourage and incentivise more advanced community pharmacy involvement in prevention activities. Further expansion of the concept may enable and incentivise community pharmacy engagement with, and contribution to, their communities. However, meaningful adoption and integration of a more person-centred approach will require a significant shift in terms of how pharmacy services are organised, reimbursed and delivered.
Dr Jayne Astbury is a Research Associate in the Division of Pharmacy and Optometry at The University of Manchester.
Professor Ellen Schafheutle is the Director of the University’s Centre for Pharmacy Workforce Studies.



Policy impacts on early medical career choices and GP retention
Dr Sharon Spooner

It is increasingly apparent that patients are finding it difficult to access health care in GP practices. There are now fewer GPs to deal with rising demands for health care, and patients are frequently diverted to a non-GP practitioner.
Among many reasons contributing to the shortfall in GPs, is the relatively low popularity of general practice as an early medical specialty choice.
By interviewing junior doctors and analysing online surveys completed by GPs, our research seeks to understand what drives GP recruitment and retention, and identify possible solutions.
Changing attitudes to specialties
The popularity of medical specialties fluctuates in response to multiple perceptions and preferences, and over recent years, societal attitudes to work and leisure have shifted.
Doctors who graduate in the UK are required to undertake two years of supervised work as part of a foundation programme, before progressing to a work-based specialty training programme which takes a further three to five (or more) years.
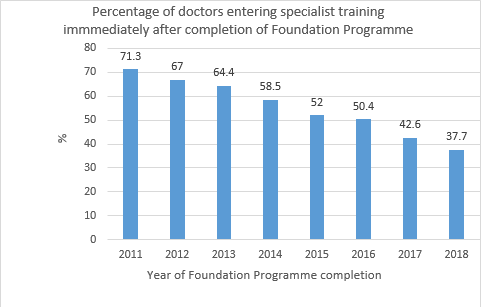
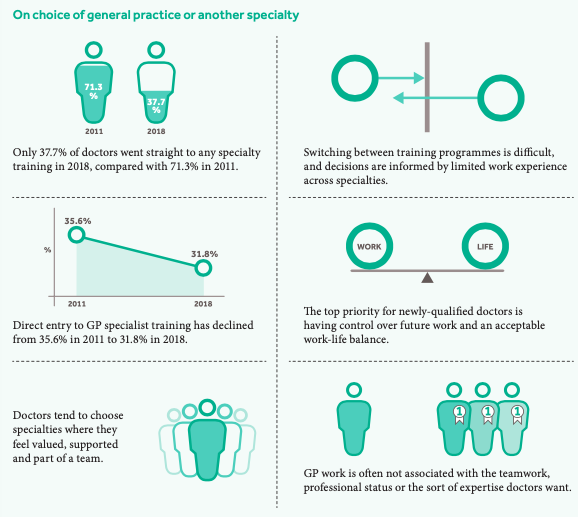
Many doctors now choose to postpone their progression to a specialty training programme.Annual official reports on training choices indicate that the proportion who directly progress has dropped drastically from 71.3% in 2011 to 37.7% in 2018.
Changing preferences regarding when they choose to enter specialty training means recruitment to training programmes is increasingly dependent on doctors resuming training in the UK at a later date. Often this is after an unspecified period when they may travel overseas, undertake career-enhancing roles, or focus on a period of recovery after two years of intense and demanding work. We do not have clear information about how many return to medical work in the UK.
What influences these early career decisions?
The inherent inflexibility of specialty training programmes means that doctors want to be sure of their decision before choosing a specialty. Each specialty training programme is constructed to prepare doctors for working in a specific specialty (or sub-specialty), making it difficult for them to switch seamlessly between different programmes. Doctors who wish to transfer between training programmes may face a salary reduction and prolong their training.
Many recently-qualified doctors are concerned about having insufficient experience of medical work to inform their choice of specialty. For many hospital specialties, it is possible for doctors to gain short-term experience of that specialty in order to assess whether they feel it suits them, before committing to several years of training.
However, apart from brief periods of closely-supervised work in general practice, there are few opportunities for doctors to find out about the realities of being a GP without formally committing to a training programme.
Apart from brief periods of closely-supervised work in general practice, there are few opportunities for doctors to find out about the realities of being a GP without formally committing to a training programme.
In addition to feeling under pressure to choose a ‘suitable’ specialty, doctors emerging from a foundation programme often report feeling exhausted and many prioritise taking control of their working lives. While providing the best quality of care remains at the core of their professional aspirations, many doctors regard work as a job rather than a definition of who they are. Time away from work is important; many reduce working hours and accept lower incomes in exchange for a better work-life balance.
What do recently-qualified doctors think?
To understand the relevance and impact of wider policy and societal issues affecting the GP workforce, researchers at The University of Manchester have been investigating the attitudes of recently-qualified doctors towards careers in general practice; the experiences and intentions of emerging GPs; and the levels of job satisfaction, job stress and intentions to quit in working GPs.

Addressing GP recruitment and retention
The evidence from these studies highlights ‘pinch points’ in the system which must be addressed if GP recruitment and retention issues are to be resolved.
It is clear that medical schools could do more to promote general practice careers. Medical schools could help provide positive experiences of general practice, where trainees get to see what motivates GPs to deliver high-quality generalist care in practices, and where continuity and patient focus are prioritised. One of the most valued aspects of work reported by established GPs is their feeling of belonging in a supportive practice team. In order to enable students to experience this, greater investment of resources is needed to select and support additional capacity within GP practices to welcome and include students as they provide longer, more meaningful placements.
GP training currently appears to be focused on clinical, rather than organisational and managerial aspects, of general practice. Lack of knowledge about GP partnership responsibilities, and concerns about future sustainability, deter many from making the longer-term commitment associated with partnership. This further undermines stability of the workforce. Because multiple organisations and bodies are involved in the delivery, assessment and regulatory monitoring of training, coordinated action is challenging.
First-hand observation or experience of general practice leads to widespread concern about unsustainably heavy workloads. This motivates many GPs at all career stages to mitigate risks of ‘burnout’ by reducing their working hours, leaving patient care (earlier in their career), or developing a more varied and manageable portfolio of work.
Evidence shows that GP workloads in practice are unsustainable due to increasingly heavy and complex caseloads, which in turn impede the resolution of inadequate recruitment and retention.
We have demonstrated that these increased workloads have also coincided with a real-term decline in GP salary of between 7%-10% per session worked, which is unlikely to stimulate recruitment.
It is important to note that current policy solutions to these issues (including the development of primary care networks) have a significant focus on broadening the mix of professionals available to provide services in practices.
However, while workforce changes designed to reduce pressure on GPs are welcomed, it is important to understand that, at present, we do not have robust evidence to show that these schemes will result in true substitution for GPs.
Indeed, it is possible that broadening the scope of available services will increase activity through supply-induced demand, and that a significant proportion of GP time will be diverted from direct patient care to training and supervising the emergent workforce.
Dr Sharon Spooner joined the Centre for Primary Care in 2014, where she is currently leading an investigation into background factors which influence the career choices of recently-qualified doctors, and is engaged in a number of projects around GP workforce and delivery of primary care.
Disclaimer
The studies cited here are funded by the National Institute for Health Research (NIHR) via the School for Primary Care Research and the Policy Research Unit in Commissioning and the Health Care System. The views expressed are those of the authors, and do not necessarily reflect those of the Policy Research Programme, NIHR, NHS England, the Department of Health, arm’s length bodies or other government departments.
Sources
‘Investigation of the factors behind the training choices of junior doctors which result in inadequate recruitment to general practice careers’. March 2017, funded by the School for Primary Care Research.
‘An investigation of factors which are associated with successful transitions from GP Specialty Training Programmes to long-term careers in NHS general practice’. October 2018, funded by the School for Primary Care Research.
‘An investigation into the career intentions and training experiences of newly qualified general practitioners’. Funded by the School for Primary Care Research.
‘National GP Worklife Survey’. Funded by the Department of Health and Social Care via the Policy Research Unit in Commissioning and the Health Care System (PRUComm) and the Department of Health and Social Care via the National Institute of Health Research Policy Research Programme.
References
1. Spooner S, Pearson E, Gibson J, Checkland K. 'How do workplaces, working practices and colleagues affect UK doctors’ career decisions? A qualitative study of junior doctors’ career decision making in the UK'. BMJ Open. 2017;7, 10, p.e018462.(10).
2. Spooner S, Fletcher E, Anderson C, Campbell JL. 'The GP workforce pipeline: increasing the flow and plugging the leaks'. British Journal of General Practice. 2018;68(670):245-6.
3. UK Foundation Programme Office. Foundation Programme Annual Report 2011.
4. UK Foundation Programme Office. F2 Career Destination Report 2018.
5. Gibson J, Rigby D, Sutton M, Spooner S, Checkland K. 'Expectations, preferences and physicians’ specialty choice'. 2018 working paper.
6. Spooner S, Laverty L, Checkland K. 'The influence of training experiences on career intentions of the future GP workforce: a qualitative study of new GPs in England'. British Journal of General Practice. 2019: bjgp19X703877.
7. Atkins R, Gibson J, Sutton M, Spooner S, Checkland K. 'Trends in general practitioner incomes in England 2008-2017: British Journal of General Practice 2020; 70 (690): e64-e70. DOI: 10.3399/bjgp19X706073.



Multidisciplinary teams in primary care
Lessons from the development of skill mix in general practice
Dr Imelda McDermott

The enduring NHS workforce crisis is caused by failure to recruit more GPs, changing demographics and complexity of patients, as well as a new generation of GPs wanting a different work-life balance.
At the same time, the emphasis in general practice is now on multidisciplinary and integrated working.
Skill mix as a solution
The policy ‘solution’ for the current workforce crisis is to broaden the skill mix in primary care, recruiting a range of different types of practitioners. There are a number of past and current policies pushing this agenda, including: clinical pharmacists in general practice; increasing the supply of physician associates (who are seen as complementary to GPs rather than a substitute); and vanguards and similar initiatives using paramedics or other clinicians to do jobs historically done by GPs.
The NHS Long Term Plan promises an increase in funding for primary and community care of at least £4.5 billion. Some of this will be used to fund expanded community multidisciplinary teams based on local GP practices that are aligned with the primary care networks (PCNs) – GP practices working together to serve populations between 30,000-50,000.
The vision for the NHS workforce, as set out in the Interim NHS People Plan, is for multiprofessional and multidisciplinary teams to be the foundation for the future. The general practice workforce will be broadened by introducing new roles such as clinical pharmacists, physician associates, paramedics, physiotherapists and social prescribers. Local GP practices and community teams will collaborate to work differently, with the intention of relieving pressures on GPs.
The vision for the NHS workforce, as set out in the Interim NHS People Plan, is for multiprofessional and multidisciplinary teams to be the foundation for the future.
Issues with the primary care workforce policy
There is a lack of clarity regarding these ‘new’ practitioners. Are they intended to be substitutes for, complementary to, or extending the scope of existing services? A BBC article calling these new practitioners ‘GP substitutes’ created a furore on social media. Clinical pharmacists have seen this as misleading and misrepresentative of the expertise that they can bring to general practice, such as face-to-face consultations for medication reviews and promoting safer use of medicine.
There aren’t enough of these practitioners to fill new roles. As part of our ongoing study exploring the scale, scope and impact of skill mix in primary care, we have mapped the composition of the primary care workforce in England.
Using the latest practice-level workforce data, we found that staff in direct patient care categories such as pharmacists, physiotherapists, physician associates and paramedics are reported relatively infrequently, and are at such low levels, they are not suitable for comparable analyses.
This highlights the limited contribution this group of practitioners is currently making to primary care. It also demonstrates the scale of expansion that would be required for them to be able to relieve pressures on GPs. Furthermore, the extent to which any or all of these practitioners undertake work as substitutes for GPs, or whether their presence generates additional GP work remains uncertain.
There is confusion over roles – what these practitioners can and cannot do. A joint report by the Health Foundation, the Nuffield Trust and The King’s Fund suggests that expanding roles requires careful articulation of roles, responsibilities and scope. There is a concern that by expanding primary care teams, GP workload could increase due to having to deal with more complex patients, rather than freeing up their time as intended.
Although it is important to define the scope of new roles, when it comes to general practice, this is problematic. General practice deals with undifferentiated and unorganised problems. Trying to categorise this work runs the risk of artificially imposing order on the inherently messy reality of general practice.
Trying to categorise this work runs the risk of artificially imposing order on the inherently messy reality of general practice.
Some of the initiatives suggested in the NHS Long Term Plan cut across previous initiatives. Practices with new practitioners in post will not benefit from new money – the only exception being pharmacists employed via the national Clinical Pharmacist in General Practice scheme or the Medicines Optimisation in Care Homes scheme.
Because the funding is only for the employment of specific new roles, there could be a mismatch between the roles that can be funded via PCNs and the roles needed by local GP practices.
Considerations for the overall policy landscape
The policy is driven, to some extent, by necessity, but it is a big assumption that these workers will reduce GP workload or relieve pressures.
It is a big assumption that these workers will reduce GP workload or relieve pressures.
There is a significant chance of supply-induced demand, as well as duplication, if patients don’t use services as intended. Patient education is therefore vital, and receptionists, acting as gatekeepers, will need to be properly trained to match patients to available appointments and the ‘right’ practitioners.
Because GPs are ultimately responsible for their patients, supervision will be required. There are some local initiatives such as the Greater Manchester Training Hub, which have started to offer training and supervision for multidisciplinary primary care teams. The Hub was developed following an investment by Health Education England North West in 2015.
Its core business is to provide placement experience for primary care staff and healthcare undergraduates through a ‘hub’ and ‘spoke’ model approach by working with local higher education institutions and general practices.
The effects of a broader skill mix in general practice are yet to be seen, and the extent to which new initiatives could reduce GP supervision workload will vary from practice to practice, and across different geographical areas and population demographics.
As part of an ongoing development of the NHS People Plan, it is more important than ever for future workforce planning to consider what local GP practices need, and think about the perspectives of staff and patients.
Dr Imelda McDermott’s research focuses on healthcare policy and the organisation of health services.



With special thanks to our contributors:
Dr Jayne Astbury is a Research Associate in the Division of Pharmacy and Optometry at The University of Manchester, where her research includes the role of role of community pharmacy in asset-based approaches.
The Rt Hon. Lord Keith Bradley is a Labour life peer who has sat under this title in the Lords since 12 June 2006. As a Member of Parliament, Lord Bradley was a member of the House of Commons Health Select Committee. As a peer, he has maintained a critical focus on health policy, including primary care, medicine, social care, with a particular commitment to improvements in mental health and learning disability services. Lord Bradley also serves as Honorary Special Adviser to The University of Manchester.
Professor Kath Checkland is a Professor of Health Policy and Primary Care at The University of Manchester, where her research explores the impact of health policy changes on the NHS. She is Co-Director of the Institute for Health Policy and Organisation. She qualified as a doctor in 1985, and continues to work one day a week as a GP.
Dr Anna Coleman is a Senior Research Fellow in The University of Manchester’s Division of Population Health, Health Services Research and Primary Care. Her research examines the impact of new practices on the NHS.
Dr Ali Hindi is a PhD researcher who has investigated the awareness, demand and use of community pharmacy services for patients with long-term conditions in the UK. He has worked on an HEE North West commissioned evaluation of non-medical prescribing in primary care, community pharmacy and mental health.
Dr Sally Jacobs is a Lecturer in Social Pharmacy at The University of Manchester. Her interests lie in organisational behaviour in health care and its influence on the community pharmacy workforce and the quality and safety of care.
Dr Imelda McDermott’s research focuses on healthcare policy and the organisation of health services. Her work also explores the interactions between academics and policymakers and the use of linguistic methods in policy analysis.
Professor Ellen Schafheutle is a pharmacist with over 20 years’ experience in health services and pharmacy practice research, with a focus on pharmacy policy, regulation and workforce. She is the Director of the University’s Centre for Pharmacy Workforce Studies.
Dr Sharon Spooner joined the Centre for Primary Care in 2014, where she is currently leading an investigation into background factors which influence the career choices of recently-qualified doctors, and is engaged in a number of projects around GP workforce and delivery of primary care. She continues to work as a part-time GP in an urban area of the West Midlands.
Dr Lynsey Warwick-Giles is a member of the Institute for Health Policy and Organisation. Her research focuses on the interaction between health policy and organisations within the health service.
Dr Sarah Willis is a Lecturer in Social Pharmacy at The University of Manchester. Her research focuses on the scholarship of teaching and learning, and the role of education and training in the development of the pharmacy workforce.
All opinions and recommendations made by article authors are made on the basis of their research evidence and experience in their fields. Evidence and further discussion can be obtained by correspondence with the authors, please contact policy@manchester.ac.uk in the first instance to arrange.
policy@manchester.ac.uk
#OnPrimaryCare
March 2020
The University of Manchester
Oxford Road, Manchester
M13 9PL


